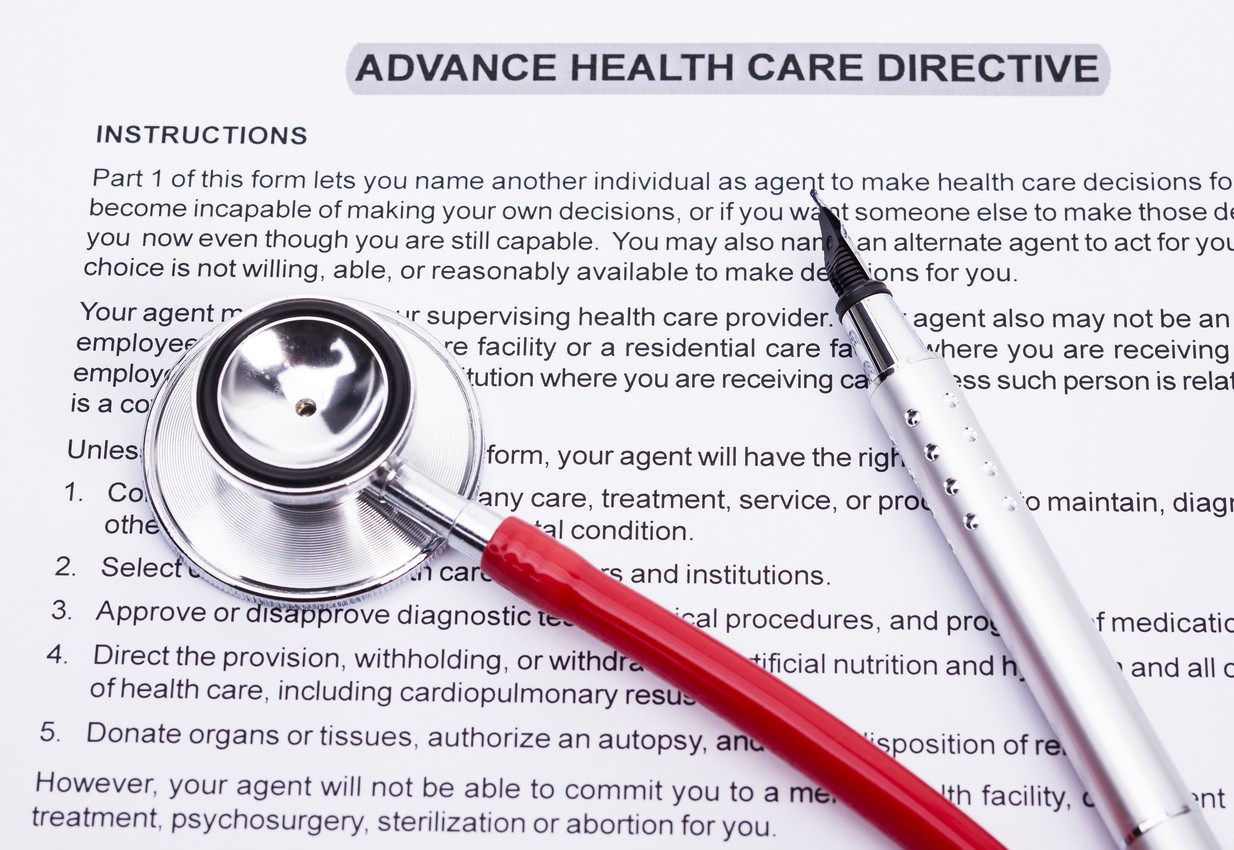
Living a long and happy life is a universal goal; But life is unpredictable. When happiness and independence are threatened by illness, injury or other life-altering medical events, everything can change very quickly. To ensure their wishes are carried out if they become incapacitated, many people are preparing advance directives that clearly state what medical care and procedures they want — and don’t want — in the event they can no longer speak for themselves. To create advance directives that will work for you when you need them, it’s important to understand what an advance directive can include, what types are legal and how to prepare yours correctly.
According to the Michigan Department of Health & Human Services, there are three main types of advance directives: Durable power of attorney for health care, a living will and a do-not-resuscitate declaration (also known as a DNR). A fourth type is a declaration of anatomical gift, which in Michigan, can also be accomplished when you renew your driver’s license. Here’s an overview of the three main advance directives.
Durable power of attorney for health care: A legally binding document, durable power of attorney for health care simply states who you choose to make medical decisions on your behalf when you no longer can, and can include both physical and mental health care decisions. The person you choose is then known as your patient advocate or your DPOA. They will be asked to begin making decisions in accordance with your preestablished wishes only after a medical professional has deemed you unable to make decisions for yourself.
If you do not define your wishes, your patient advocate must then make decisions in your best interest. If you do define your wishes, you choose what decisions your patient advocate can make for you, including how to pay for your care. You may also choose a second patient advocate to serve in the event your first choice is unable to, but by law, only one can serve at a time. This document must be written, signed by you and witnessed by two adults who are not related to you, not the patient advocate and not employed at a health care facility where you are or will be treated. To be legally binding, your patient advocate must also sign an acceptance document.
Living will: In the event you become “terminally ill or permanently unconscious,” a living will can dictate your medical care wishes. Unlike a DPOA which can be used during times of temporary impairment, a living will essentially provides your family and medical professionals with your final wishes concerning the level of care you want to receive. Living wills are not legally binding in Michigan, but they remain one way to let your wishes be known, and should be written, signed and witnessed by two adults unrelated to you.
Do-not-resuscitate order: In the event that your heart and lungs cease to function, you can choose to forego resuscitation through a do-not resuscitate order. DNRs are legally binding in Michigan and can include specific wishes such as instructing care givers or others not to call 911 if you stop breathing. Again, a DNR should be written, signed by you and your physician, and witnessed by two adults. You can also provide your patient advocate with the authority to sign a DNR for you. In addition to a DNR, you may also have a do-not-intubate order or DNI if you do not wish to be on a mechanical ventilator.
All of these advance directives are voluntary and can be revoked at any time regardless of your physical or mental health status. You can also change your mind about earlier treatment decisions without revoking the documents by communicating your wishes in any way. If you do change your mind, it is best to destroy the old documents and create new ones that agree with those changes.
If you decide to complete one or more advance directives, take time to consult with your family, your physician, your spiritual advisor, and your intended patient advocate so that everyone is clear about what you want, don’t want, and when. The Mayo Clinic article, “Living wills and advance directives for medical decisions,” looks at some of the possible medical treatments to consider. You can also include your choice for burial or cremation and other end-of-life decisions that will state exactly what level of palliative care you desire such as whether you prefer to be at home or in hospice. The University of Michigan offers a checklist and other decision-making tools for advance directives in the document, “Start the Conversation: Making your health care wishes known.” Forms and other detailed information for DPOA and DNR orders are available in the MDHHS document “Advance Directives Planning for Medical Care in the Event of Loss of Decision-Making Ability.”
After you complete your advance directive, make copies and provide one to your physician and to your patient advocate. You may also give copies to family members to ensure everyone is informed. It’s a good idea to keep a list of everyone who has a copy to avoid conflicts if you make changes or revoke your advance directive. In the event you enter a health care facility, be prepared to provide a copy of your advance directive for your medical file. You may also want to carry a wallet card stating that you have an advance directive. Also review your advance directive at least annually to be sure you still agree with your original decisions.
Advance directives take time and careful thought, but are well worth it during an emergency, illness or end-of-life crisis. By making your wishes known to your loved ones now, you relieve them of having to guess at what you would want, and minimize the possibility that the wrong decisions are made on your behalf. Most of all, an advance directive will help provide those you care about most with peace of mind during difficult times.